Thyroid Series: Hyperthyroidism and Solutions Part #1

Welcome to our Thyroid Series of blog articles. This article covers hyperthyroidism and how to address it using Functional Medicine and diet. Next week we will discuss other FM approaches to hyperthyroidism. In our Thyroid Series, we cover the basics on the thyroid here and hypothyroidism here and here. In future thyroid series articles, we will look at other conditions of the thyroid and how to address each one. We hope you will stay with us and follow the series week by week.
** Please note: If you want the short summary version of this article with a video, then please click here
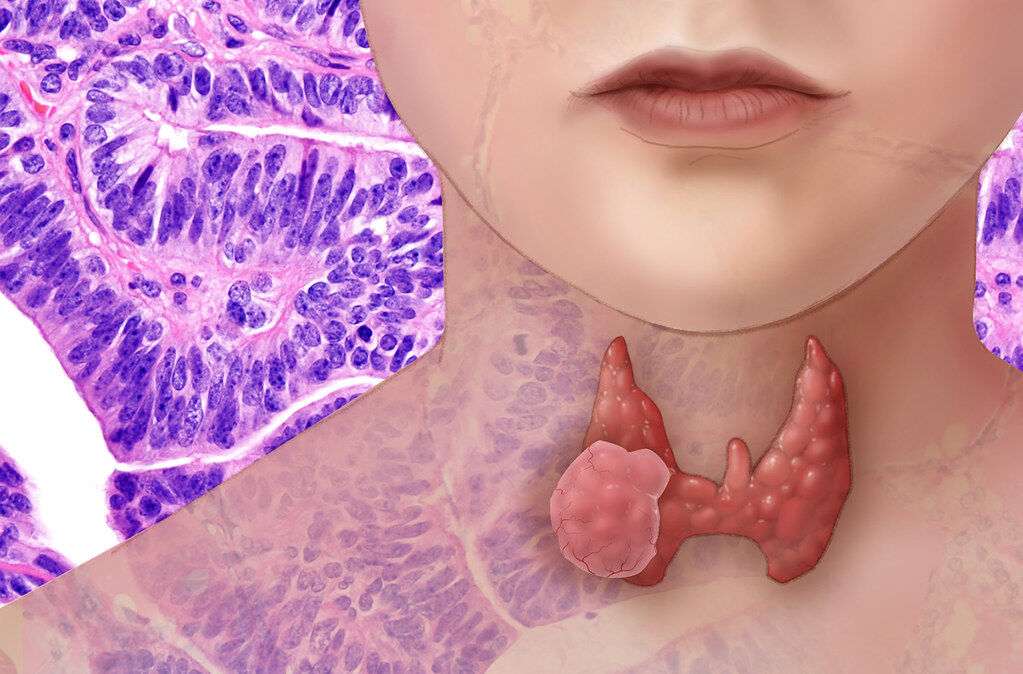
Hyperthyroidism: What is it?
Hyperthyroidism, or overactive thyroid, is when the thyroid produces too much thyroid hormones. Thyroid hormones regulate multiple functions in the body; how the body uses energy, consumes oxygen and produces heat (The Endocrine Society, 2019). Thyroid hormones affect nearly every organ in the body, including how the heart beats. The main thyroid hormones are T3 and T4.
Women are 2 to 10 times more likely than men to develop hyperthyroidism (National Institutes of Health, 2016). 1.2% of people in the US have hyperthyroidism, which is approximately 1 person out of 100. ( National Institute of Health, 2016) Hyperthyroidism is less common than underactive thyroid or hypothyroidism.
Symptoms of Hyperthyroidism
Thyroid hormones control metabolism, which runs the pace of body processes. If there is too much thyroid hormones, the body speeds up. This is reflected in the symptoms of hyperthyroidism (American Thyroid Association, 2020).
- Nervousness, anxiety, irritability
- Increased sweating
- Heart racing, fast or uneven heartbeat or palpitations (pounding in the heart)
- Hand tremors: shaking in hands and fingers
- Mood swings
- Difficulty sleeping
- Thinning skin
- Fine, brittle hair
- Weakness in muscles, especially in the upper arms and thighs
- Many people initially have a lot of energy. But as time goes on the body tends to break down, so being tired becomes very common
- Sensitivity to heat
- A swollen thyroid (called a goiter), swelling at the base of your neck
- Losing weight suddenly, without trying
- Having more bowel movements and diarrhea is not common
- Changes in menstrual cycle, menstrual flow may lighten and menstrual periods may occur less often
Untreated hyperthyroidism can cause serious problems with the heart, bones, muscles, menstrual cycle, and fertility (National Institutes of Health, 2016).
Hyperthyroidism Causes
- Graves’ disease: This autoimmune disorder is the most common cause of hyperthyroidism in more than 70% of people who have hyperthyroidism (American Thyroid Association, 2020). Grave’s is overproduction of thyroid hormone by the entire thyroid gland. It is caused by antibodies in the blood that turn on the thyroid and cause it to grow and secrete too much thyroid hormone (American Thyroid Association, 2020). It is important to identify the root cause(s) of Grave’s disease, and focus on gut healing given it is an autoimmune condition. We will cover Grave’s in more detail in a future blog.
- Thyroid nodules: Thyroid nodules are lumps on the thyroid. They are common and usually benign. Sometimes one or more nodules may become overactive and produce too much thyroid hormone (National Institutes of Health, 2016). Having many overactive nodules occurs most often in older people (National Institutes of Health, 2016). Again, it is important to identify and address the root cause(s) of thyroid nodules, which is a topic for a future blog in our thyroid series.
- Thyroiditis: This is inflammation of the thyroid, often caused by a problem with the immune system or a viral infection. The thyroid swells and leaks hormones so that there are excess thyroid hormones in the blood (American Thyroid Association, 2020). It is often caused by an infection (Epstein-Barr Virus, Lyme disease or other bacterial or viral infections). The infection affects thyroid function, possibly causing thyroiditis and altering the production of thyroid hormones (American Thyroid Association, 2020). It is important to find the source of the inflammation and/ or address the infection.
- Postpartum thyroiditis: Thyroiditis can develop after a woman gives birth (National Institutes of Health, 2016). This condition can be autoimmune. It is important to find out the root cause(s) and to address them.
- Excess medication: Taking too much exogenous thyroid hormone will cause excessive thyroid hormones (American Thyroid Association, 2020). There is excess thyroid hormone but the thyroid is not overactive. It is important to work with a doctor to get medication dosages right.
- Excess iodine: The thyroid uses iodine to make thyroid hormone. The amount of iodine consumed affects the amount of thyroid hormone the thyroid will make. Hyperthyroidism can be caused by too much iodine in the diet. Some medicines, for example the heart medicine amiodarone, and cough syrups, may contain a lot of iodine (National Institutes of Health, 2016). Interestingly, excessive iodine can also exacerbate Hashimoto’s, another thyroid autoimmune condition that usually causes low thyroid or hypothyroidism. Hashimoto’s can cause thyroid to alternate in some cases between hypo (low) thyroid and hyper (high) thyroid but the general tendency is towards hypothyroid (or low). Oddly enough, in some cases, iodine can slow thyroid hormone production and also reduce the activity of an overactive thyroid gland. One conventional medical treatment for hyperthyroid involves using a radioactive iodine to intentionally destroy part of the thyroid gland in order to slow production of thyroid hormone (more on this later). This, of course, is highly invasive and we will review natural methods to get to the root cause of excessive thyroid hormone without destroying the thyroid gland.
To Read About Blog Topic, Scroll Down
Want To Work With Our Clinic?
Do you have a chronic or mystery illness that no one has been able to help you with? Are you simply wanting to re-connect with a healthier version of yourself? It’s Time To Finally Feel Better!
Other Root Causes
- Gluten: As we have mentioned in our two previous articles on the thyroid (here and here) it is best to avoid gluten for two reasons. Firstly, gluten contributes to leaky gut. Once leaky gut is present, then unwanted substances can escape from the gut into the bloodstream. This can over-activate the immune system and potentially lead to autoimmunity. Secondly, the gluten molecule is very similar in structure to thyroid tissue. If gluten is able to get into the bloodstream and circulate, it can cause the immune system to mount an attack. Due to the molecular mimicry between gluten and thyroid tissue, this may end up being an attack on the thyroid itself.
- Mercury: The thyroid is very sensitive to toxins. Mercury is an environmental toxic metal found in the general environment. It can cause detrimental effects to the thyroid gland (Khan R, 2019). One study on tadpoles found that high dose mercury damaged thyroid, disrupted thyroid function and liver cell structures and altered gene expression (Shi Q, 2018). For humans, the health impact of exposure to mercury is due more to chronic, low or moderate grade exposure and not necessarily a high concentration exposure (Ye BJ, 2016). Sources of potential mercury exposure include vaccines, dental amalgams, breathing contaminated air, drinking contaminated water or eating contaminated food, particularly mercury contaminated fish.
- Leaky gut / Gut health: As with most conditions that we write about, it is imperative to address gut health. There are many GI issues that can affect the thyroid, particularly leaky gut. The composition of the gut bacteria also plays an important role in thyroid function (Fröhlich E, 2019). Dysbiosis, or an imbalanced gut microbiome, is emerging as a key issue in people with thyroid disorders (Fröhlich E, 2019). Small Intestinal Bacterial Overgrowth (SIBO) has been linked with thyroid issues (both as a cause and a result of thyroid problems).
- Infections such as Epstein-Barr Virus, Lyme disease or other bacterial or viral infections: Inflammation of the thyroid gland can occur as a result of a (typically viral) infection (EndocrineWeb, 2014). The infection can affect thyroid function, possibly cause thyroiditis and alter the production of thyroid hormones (American Thyroid Association, 2020). Gut infections like Helicobacter pylori have also been linked with thyroid antibody formation and clearing this infection may lower thyroid antibodies in some people (Salami MA, 2013).
- Inflammation: Inflammation of the thyroid is thyroiditis. It is important to find the source of the inflammation, which could be due to a viral infection, autoimmunity, inflammatory diet, or other root cause. FM will help to identify and address inflammation.
The Standard Medical Treatment for Hyperthyroidism:
In standard conventional treatment, Medication is frequently used with hyperthyroidism:
- Anti-thyroid drugs: These drugs are commonly prescribed for hyperthyroidism. They block the thyroid gland from making new thyroid hormone. Side effects include allergic reactions in about 5% of patients who take them (American Thyroid Association, 2020). Very rarely (1 in 500 patients) there is a serious side effect in which the number of white blood cells decrease, lowering resistance to infection (American Thyroid Association, 2020).
- Beta-blockers: Beta blockers do not block thyroid hormone production, but reduce symptoms until other treatments take effect. They can relieve symptoms such as tremors, rapid heartbeat, and nervousness or anxiety (American Thyroid Association, 2020).
Radioactive iodine:
Over 70% of adults who develop hyperthyroidism are treated with radioactive iodine (American Thyroid Association, 2020). In this treatment, the patient takes a small amount of radioactive iodine. Thyroid cells need iodine to make thyroid hormone so these cells take up the radioactive iodine (American Thyroid Association, 2020). It destroys the cells that have taken it up, shrinking the thyroid or thyroid nodules and the level of thyroid hormone in the blood returns to normal (American Thyroid Association, 2020).
Almost everyone who has radioactive iodine treatment later develops hypothyroidism because the thyroid hormone-producing cells get destroyed (National Institutes of Health, 2016). Hypothyroidism is considered easier to treat and causes fewer health problems than hyperthyroidism in the long run. People with hypothyroidism are left to control the condition with daily thyroid hormone medicine (National Institutes of Health, 2016).
Surgery:
The least common treatment for hyperthyroidism is thyroidectomy, surgery to remove part or all of the thyroid gland (National Institutes of Health, 2016). When part of the thyroid is removed, thyroid hormone levels may return to normal (National Institutes of Health, 2016). It is possible to still develop hypothyroidism after surgery (National Institutes of Health, 2016). In this case, the patient will need to take thyroid hormone medicine. If the whole thyroid is removed, it will be necessary to take thyroid hormone medicine for life (American Thyroid Association, 2020).
Functional Medicine Solutions to Hyperthyroidism:
There are also many non-pharmaceutical solutions that can address hyperthyroidism. It is best to work with a FM practitioner to assess your case and decide on the best protocol for you, as sometimes medications are helpful or even necessary.
Many of these steps can be taken simultaneously. The most obvious are:
DIET:
Foods to avoid:
High-iodine foods: It is important to avoid consuming excessive levels of iodine with hyperthyroidism. Iodine is used by the thyroid to make thyroid hormones so consuming too much iodine can cause an over-production of thyroid hormones. This can worsen a hyperthyroid condition. It is possible that a skilled functional medicine practitioner may use iodine very carefully as part of a treatment plan for hyperthyroidism, but this is best left for professional guidance.
High iodine foods to avoid are:
- Sea vegetables: Kelp is rich in iodine as is dulse, nori or other kinds of seaweed
- Seafood: Shrimp, scallops, crab, oysters, etc.
- Fish, especially from saltwater: Cod, tuna, canned salmon, sushi
- Iodized salt: Iodine is added to salt. It is better to consume less-processed pink Himalayan salt or sea salt (although these options still do contain some iodine)
- Dairy products: These are typically enriched with iodine so avoid cheese, milk, yogurt, ice cream, etc.
- Eggs
- Prunes
- Iodine supplements can have the same impact as eating too much iodine
Gluten: Gluten is an issue for gut health and can lead to intestinal permeability. We have discussed this here. In addition, gluten is likely to cause inflammation to the thyroid (Wong, 2017). Gliadin, a component in gluten, looks like transglutaminase, an enzyme found in the body, including in the thyroid (Wong, 2017). Once gliadin escapes the GI tract through a leaky gut, the body’s antibodies may attack both the gliadin and transglutaminase (Wong, 2017). So, the thyroid gland is potentially under attack whenever gliadin is in the blood stream (Wong, 2017). This is why it is so important to go gluten-free with a thyroid condition (Wong, 2017).
Nitrates: Processed meats (cured meats, sausage, bacon, ham, salami, corned beef, hot dogs, smoked salmon, dried fish and jerky) contain nitrates to preserve them and make them last longer. Nitrates compete with iodine uptake by the thyroid, potentially affecting thyroid function (Ward MH, 2010). Nitrates can also be found as a contaminant of drinking water in agricultural areas and is found in some vegetables (Ward MH, 2010).
Caffeine: Caffeine can lead to increased anxiety, nervousness, irritability, tremors and rapid heart rate in anyone, especially if taken to excess. If caffeine has this effect on a hyperthyroid patient, then it is best to avoid or limit caffeine-containing foods and drinks. This includes coffee, tea, soda and chocolate, which can all can exacerbate the symptoms of hyperthyroidism.
It is also advisable to avoid inflammatory foods like processed, packaged, fast or junk foods, excess sugar and vegetable & seed oils. Please see our article on Hypothyroidism for an explanation of the impact of these foods.
OK, so what do you eat for hyperthyroidism?
We recommend following a whole-foods based, blood sugar-balancing, anti-inflammatory diet. Examples are the Paleo diet or a gluten-free Mediterranean diet.
In addition, specific foods should be eaten to help thyroid function:
Eat a low-iodine diet. Hyperthyroidism is quite common among cats and there are many studies on hyperthyroid cats. One study fed a restricted-iodine diet to cats which reduced T4 levels to within reference range, while improving some symptoms (Hui TY, 2015). This was for the majority of cats with hyperthyroidism in the study (Hui TY, 2015).
Low iodine foods include:
- Non-iodized salt
- Fresh and frozen vegetables in cooked or raw form
- Unprocessed meats, including beef, pork and poultry
- Rice
- Egg whites
- Fresh fruit
- Unsalted nuts
- Unsalted nut butters such as peanut butter and almond butter
- Dark, non-dairy chocolate
Get adequate selenium. Selenium is important for healthy thyroid function (Köhrle, 2015). Research indicates that taking selenium for both low thyroid and overactive thyroid conditions improves clinical scores and well-being of patients (Köhrle, 2015). Good sources of selenium include Brazil nuts, tuna, ham, beef, turkey and chicken.
Eat cruciferous vegetables (with a caveat). Broccoli, kale, cabbage, Brussels sprouts, and other cruciferous vegetables contain goitrogens. Goitrogens inhibit thyroid function. Contrary to what we do with hypothyroidism, eating cruciferous vegetables can help in the case of hyperthyroid as they will slightly depress thyroid function. Eat cruciferous vegetables raw or only slightly cooked to maximize goitrogenic activity (McMillan M, 1986). If there is swelling in the thyroid gland or history of goiter or iodine levels get too low, it is best to avoid or limit goitrogenic foods or work with a skilled practitioner to balance iodine needs, benefits from goitrogenic foods, and consistent measurements of thyroid hormone to make adjustments as needed.
** Please check our blog next week to read our next article in the Thyroid Series on **
Hyperthyroidism & Solutions using Functional Medicine Part #2
Are You Suffering From A Chronic Illness?
Does your current health situation look like this…
- Do you feel that you have tried many things and either nothing works, or the treatment does not hold?
- Have you been told that there is nothing that can be done to reverse your illness and you just need to manage symptoms?
- Does your illness impact your work, your family, your happiness and your social life?
We specialize in finding answers and solutions for complicated chronic illness when people feel like they have tried everything. If this sounds like you, book a free call with us to see if we are the right fit for your health goals.
Dr. Miles has spoken for the following organizations:
















Responses