Symptoms of Lyme Disease in Humans

In this blog, we will look at the symptoms of long-term Lyme Disease in Humans. You will learn:
- What chronic or long-term Lyme Disease is
- What the symptoms of long-term Lyme Disease are
- How Functional Medicine can help with long-term Lyme
Do you suffer from pain, fatigue or difficulty thinking? Do you have long-term Lyme Disease and do you know how to recognize it? Then this blog is for you. Please read on for the details!
** Please note: If you want the longer, more detailed version of this article, then please click here **
To Read About Blog Topic, Scroll Down
Want To Work With Our Clinic?
Do you have a chronic or mystery illness that no one has been able to help you with? Are you simply wanting to re-connect with a healthier version of yourself? It’s Time To Finally Feel Better!
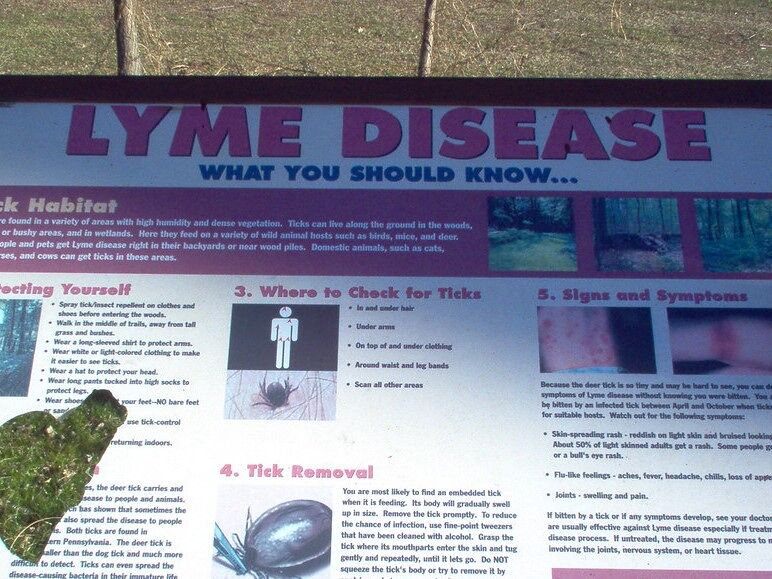
Lyme Disease is a bacterial infection, caused by Borrelia burgdorferi. Borrelia is a bacterium that is transmitted by an infected black-legged tick, most commonly spread by a tick bite. We have written extensively about Lyme Disease in our blog. Start here with our blog on ‘What is Lyme Disease’?
Lyme is a complex disease with both acute and potentially chronic symptoms. It typically, but not always, starts with a rash, headache, fever and chills. It can further develop into more serious symptoms such as possible arthritis, neurological or cardiac issues.
Unfortunately, Lyme Disease is not completely understood in the medical world. It is often missed or misdiagnosed. When left untreated in its acute early phase, it can become chronic. Sometimes, treatment fails and it can still become chronic Lyme. Sometimes, a person goes undiagnosed for Lyme because they didn’t notice the tick bite and never went to the doctor. In all of these scenarios, a person can develop chronic long-term symptoms that will likely very much affect their quality of life.
Symptoms of Lyme Disease in Humans: Different Types of Long-term Lyme Disease Exist: Chronic Lyme Disease vs. PTLDS
Chronic Lyme Disease and Post-Treatment Lyme Disease Syndrome (PTLDS) are two terms that are sometimes used to describe very similar conditions. Strictly speaking, PTLDS refers to people who were already treated for Lyme Disease but, unfortunately, go on to experience longer lasting Lyme Disease symptoms. It does not include those who received a misdiagnosis or a delayed diagnosis, which then resulted in chronic symptoms of Lyme Disease before receiving any treatment for Lyme. That is defined as chronic Lyme Disease.
It’s a little confusing but the bottom line is that people with either PTLDS or chronic Lyme are still suffering from Lyme symptoms, have a reduced quality of life and are probably not getting the medical help they need. This is where Functional Medicine, and our clinic in particular, can help. Please get in touch with us if you are struggling with ongoing issues from Lyme Disease here.
Symptoms of Lyme Disease in Humans: What are the Symptoms of Lyme and Long-term Lyme Disease?
We have covered Lyme symptoms before in other blogs on Lyme, which you can find on our blog page here. But we will review the symptoms here to emphasize the difference between symptoms of acute early-stage Lyme and the long-term symptoms that Lyme can manifest.
The early-stage symptoms of Lyme typically appear 3 to 30 days after exposure and most commonly include:
- Fever
- Chills
- Headache
- Fatigue
- Muscle pain
- Joint pain and swelling
- Swelling of the lymph nodes
- Erythema migrans (EM), the bull’s-eye-shaped rash at the site of the tick bite
The EM bulls-eye rash is the typical Lyme Disease symptom. It shows up at the site of the tick bite within 1–3 weeks (Schmid H, 2021). It clears within a few days to weeks. This rash appears in 70%-80% of people infected with Lyme (CDC, 2021). We see it less often in our clinical experience.
Not everyone gets the bull’s-eye rash, which can make Lyme harder to diagnose. Another complication is that up to 30% of patients don’t remember getting a bull’s-eye EM rash (CDC, 2021). The CDC has reported that less than 50% of patients recall a tick bite or develop the signature bull’s-eye rash (CDC, 2007). To make things worse, the routine Lyme screening test has up to 60% false negativity (CDC, 2007).
Given these circumstances, it can easily be that a person doesn’t get a bull’s-eye rash or doesn’t notice they were bitten by a tick. So, they don’t go to see a doctor. Or they don’t mention it to the doctor and the doctor doesn’t look for Lyme in the person.
Symptoms of Lyme Disease in Humans: Symptoms of Late-stage, Chronic Lyme or PTLDS
Late-stage Lyme Disease has different symptoms. These may appear months after the initial tick bite and may include:
- Severe headaches and neck stiffness
- Additional EM rashes in new places on the body
- Facial palsy, also known as Bell’s palsy – paralysis of one side of the face
- Arthritis or joint pain and swelling, especially of large joints, such as the knee
- Tendon, muscle, joint, nerve or bone pain
- Dizziness or shortness of breath
- Inflammation of the brain or spinal cord
- Shooting pains, numbness or tingling in the hands or feet
- Fatigue
- Fevers, chills and sweats
- Chronic inflammation
- Tremors
- Respiratory infections
- Sore throat
- Stomach pain
- Heart palpitations and irregular heartbeat
- Anxiety and paranoia
- Rage
- Hallucinations
- Hearing sensitivity
- Vocal cord damage
- New food allergies or multiple-chemical sensitivities
- Seizures
- Cardiac issues or Lyme carditis (inflammation of the heart)
- Cognitive neurological issues
- Alzheimer’s Disease (you can read more about Lyme & Alzheimer’s in our blog here)
- Immune system dysfunction and general inflammation
- Inflammation of the lining of the brain or meninges
- Stress, anxiety and depression can result from being ill for so long, from being misdiagnosed or from the severity of symptoms
That’s quite a long and scary list of possible symptoms. This is why early detection is key. Lyme Disease is easiest to treat at the early or acute stage, within the first 30 days of exposure.
Symptoms of Lyme Disease in Humans: How Common is Lyme Disease and Does it Often become Long-term, Chronic or PTLDS?
The true incidence of Lyme is thought to be higher than the medical statistics reflect. Rates vary around 10%, depending on the population studied (Schmid H, 2021). PTLDS is estimated to affect 1.5 million people in the US, a significantly higher figure than the 300,000 that the CDC reports (DeLong A, 2019).
Diagnosing Lyme Disease can be challenging. It is called The Great Imitator. It can mimic many other conditions. This often leads to misdiagnosis. It can be mistaken for juvenile arthritis, multiple sclerosis, neuropsychiatric disorders and Alzheimer’s Disease.
As mentioned, untreated Lyme Disease can become chronic Lyme. It can also progress and develop into these other conditions. This makes the ‘misdiagnosis’ partially correct, even though the root cause of the disease was not identified correctly at the time of diagnosis.
It is also challenging to get correct and current statistics on Lyme, due to the frequent misdiagnoses or doctors just missing it entirely. The best available statistics show that:
- An estimated 5-20% of patients may have chronic symptoms after getting Lyme Disease and these symptoms can be debilitating (Columbia University, 2021).
- 5%–10% of patients had persisting symptoms 6–12 months after antibiotic treatment for Lyme Disease (Schmid H, 2021). Most of these symptoms were unspecific but match PTLDS symptoms (Schmid H, 2021).
- Up to 15-40% of late-stage Lyme patients develop neurological disorders, which are responsible for many symptoms of chronic Lyme Disease (CDC, 2007).
Symptoms of Lyme Disease in Humans: Does Treatment for Lyme Work?
The treatment failure rate for all stages of Lyme Disease is quite high. According to the CDC, as many as 20% of patients remain ill after the short-term treatment protocol recommended by the IDSA, The Infectious Diseases Society of America.
Other studies suggest the treatment failure rate for early Lyme Disease may be as high as 36% (Aucott JN, 2013).
In late Lyme Disease, treatment failure rates may exceed 50% (Johnson L, 2004). A number of studies have found treatment failure rates ranging from 24 to 50% for the standard protocols of intravenous antibiotics for 2 to 4 weeks or oral antibiotics for 4 weeks (Johnson L, 2004).
One study found that 25% of patients suffer from residual neurological symptoms 5 years post-treatment (Berglund J, 2002).
Symptoms of Lyme Disease in Humans: Integrative Treatment for Chronic Lyme Disease
Early diagnosis and treatment are very important in avoiding long term symptoms (Berglund J, 2002). At later or chronic stages, Lyme Disease becomes harder to treat with antibiotics alone.
If someone has progressed to chronic later stage Lyme, or develops post-treatment Lyme, more or extra antibiotics is not a successful treatment and can be harmful (Schmid H, 2021). Sometimes there isn’t proof of an ongoing bacterial infection, so repeated or longer antibiotic treatment will not help and can harm the gut microbiome (Schmid H, 2021).
Long lasting symptoms may require a more comprehensive and functional approach including diet, supplements, herbs and lifestyle changes, especially when the disease has developed into neurological or psychiatric symptoms. This is where Functional Medicine becomes your best option.
In our Functional Medicine Clinic, we are Lyme-literate experts and we use a natural full-spectrum approach to cure Lyme Disease. This involves digging deep, looking for the root causes and using a variety of healing approaches, not simply relying on more antibiotics.
If you are interested in the science and why Lyme can develop into a chronic condition…. Read on for more info!
Symptoms of Lyme Disease in Humans Why do People Develop Chronic Lyme or PTLDS?
Experts don’t know for sure why some people experience persistent symptoms, even with treatment (Schmid H, 2021).
Some theories to explain long-term Lyme include:
- The Borrelia burgdorferi infection may trigger an autoimmune response that causes symptoms that last, even after the infection has been cleared (Columbia University, 2021). Autoimmune responses and syndromes can happen after other types of infections, such as campylobacter leading to Guillain-Barré syndrome, chlamydia leading to reactive arthritis and strep throat leading to rheumatic heart disease (CDC, 2022) and (Columbia University, 2021).
- Some experts think that PTLDS is due to a persistent but very difficult to detect infection (CDC, 2022) and (Columbia University, 2021). The bacteria can remain dormant in the body and can survive high dose antibiotics (Rudenko N, 2019).
- Biofilms are also an explanation. In Borrelia, biofilms can form to protect the bacteria. These dormant bacterial cells can hide in biofilm and survive the standard antibiotic treatment and then be reactivated (Rudenko N, 2019).
- It could be that the symptoms of PTLDS are due to other root causes and are unrelated to the initial Borrelia burgdorferi infection (CDC, 2022).
- There could be damage from the prior infection or even changes in brain chemistry, leading to abnormally activated pain or mood pathways or altered cognition (Columbia University, 2021).
Symptoms of Lyme Disease in Humans: How Functional Medicine can help with Chronic Lyme or PTLDS
Diagnosing PTLDS can be a challenge (Schmid H, 2021). PTLDS is a diagnosis of exclusion where we rule out other diseases. In our clinic, we conduct a detailed analysis and search for the root causes of the symptoms. Then FM principles can be applied to address the root cause issues to improve symptoms, especially if no treatable diagnosis has been found.
In our clinic, we have expertise in treating a range of complicated, difficult-to-diagnose conditions like chronic or Post Treatment Lyme Disease Syndrome. We regularly treat and resolve Lyme, chronic infections and other complex conditions in patients in our Functional Medicine clinic.
** Please stay tuned for our next Blog! **
Are You Suffering From A Chronic Illness?
Does your current health situation look like this…
- Do you feel that you have tried many things and either nothing works, or the treatment does not hold?
- Have you been told that there is nothing that can be done to reverse your illness and you just need to manage symptoms?
- Does your illness impact your work, your family, your happiness and your social life?
We specialize in finding answers and solutions for complicated chronic illness when people feel like they have tried everything. If this sounds like you, book a free call with us to see if we are the right fit for your health goals.
Dr. Miles has spoken for the following organizations: