PCOS: Polycystic Ovarian Syndrome, Part #1: The Causes of PCOS
This week, we discuss the causes of PCOS Next week, please read on for our article on the solutions to PCOS.
WHAT IS PCOS?
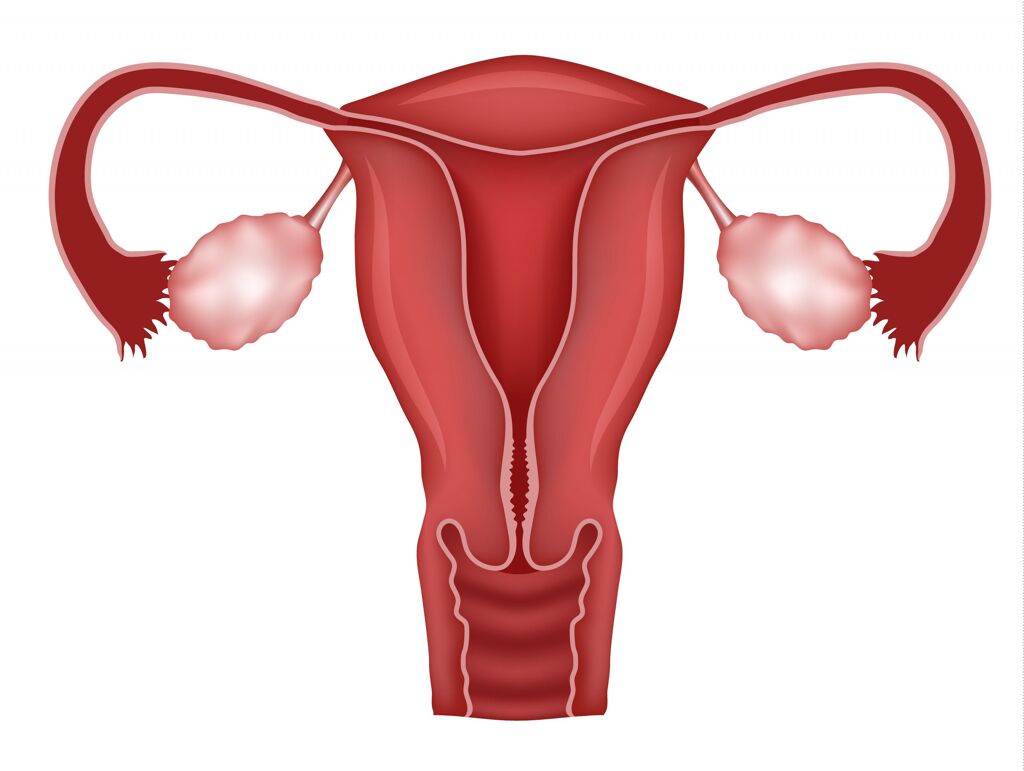
Polycystic ovary syndrome (PCOS) is a hormonal imbalance that affects women. It involves reproductive and hormonal disturbances, primarily anovulation (when a woman does not ovulate) and high levels of androgen or male hormones in women (Diamanti-Kandarakis E, 2012). Hormonal issues are typically accompanied by metabolic disturbances such as increased blood pressure, high blood sugar, insulin resistance, excess body fat around the waist and abnormal cholesterol or triglyceride levels (Diamanti-Kandarakis E, 2012).
It is estimated to affect 2–20% of reproductive-aged women (Pourteymour Fard Tabrizi F, 2020). This, of course, is a massive range, largely because PCOS goes undiagnosed in so many cases. Many clinicians report at least half of infertility cases in women involve PCOS.
PCOS can lead to an increased risk of developing several medical complications including:
- Insulin resistance
- Type 2 diabetes
- High cholesterol
- High blood pressure
- Heart disease
- Stroke
- Sleep apnea
- Possibly an increased risk of endometrial cancer (Roos N, 2011)
SYMPTOMS of PCOS include:
- Irregular periods or no periods at all
- Heavy periods
- Pelvic pain
- Cysts on the ovaries
- Difficulty getting pregnant (because of irregular ovulation or failure to ovulate)
- Insulin resistance
- High testosterone which can cause excessive hair growth (hirsutism) – usually on the face, chest, back or buttocks
- Weight gain
- Thinning hair and hair loss from the head
- Oily skin or acne
- Patches of thick, darker, velvety skin on the neck, arms, breasts or thighs
- Anxiety or depression
- Sleep apnea
To Read About Blog Topic, Scroll Down
Want To Work With Our Clinic?
Do you have a chronic or mystery illness that no one has been able to help you with? Are you simply wanting to re-connect with a healthier version of yourself? It’s Time To Finally Feel Better!
KEY RISK FACTORS (some of the causes of PCOS)
- Obesity is a risk factor for PCOS (Kakoly NS, 2019). One study found that 60% of women with PCOS are obese (Roos N, 2011).
- Gut dysbiosis and leaky gut: We will cover this issue in greater detail below
- Metabolic syndrome: a set of conditions that include increased blood pressure, high blood sugar / insulin resistance, excess body fat around the waist and abnormal cholesterol or triglyceride levels. These often occur together and increase risk of heart disease, stroke and type 2 diabetes.
CAUSES OF PCOS
The specific cause of PCOS is unknown.
It is a multifactorial disorder mainly brought on by genetic and environmental factors (Zhang F, 2019). It is thought that high levels of male hormones or androgens prevent the ovaries from producing hormones and making eggs normally (Pourteymour Fard Tabrizi F, 2020). Genes, insulin resistance and inflammation have all been linked to excess androgen production.
The best current understanding of the biochemistry involves the 17,20-lyase enzyme (Keleştimur F, 1999). This enzyme is secreted by the adrenal glands. 17,20-lyase helps with the conversion of cholesterol to the androgen hormones testosterone and DHEA (Keleştimur F, 1999). Then aromatase enzyme converts some of that testosterone into estrogen (Keleştimur F, 1999).
Because 17,20-lyase is upregulated with PCOS and is involved with producing testosterone and DHEA, it makes sense that in lab reports for individuals with PCOS, we often see elevated testosterone and/or DHEA-S in the blood (Keleştimur F, 1999). There can also be estrogen dominance because some of the excessive testosterone is getting converted into estrogen with the aromatase enzyme. When estrogen, in relationship to progesterone, becomes proportionately elevated, we can see symptoms associated with estrogen dominance.
Insulin resistance (and/or hyperinsulinemia) -> 17,20-lyase enzyme upregulation -> increased testosterone and DHEA -> potential for increased estrogen from aromatase enzyme converting more testosterone into estrogen
Interactions between genetic, behavioral and environmental factors are involved in the development of PCOS so epigenetic (environment and lifestyle) factors are of prime importance (Pourteymour Fard Tabrizi F, 2020). Some researchers think that it manifests largely due to poor lifestyle habits (Patel, 2018).
THE FIVE CONTRIBUTING FACTORS TO PCOS (partially are causes of PCOS)
- Diet:
Diet is the major environmental factor in developing PCOS (Diamanti-Kandarakis E, 2012). Excess calories leading to obesity is widely recognized to have an aggravating impact. Obese women with PCOS treated with a 1,000 kcal diet for 6–7 months showed body weight loss of 5–10% and improvements in their health including renewed ovulation, increasing pregnancy rate and lower levels of insulin and androgens (Zhang F, 2019).
It is well-established that excessive sugar and refined carbohydrates in the diet contribute to many of the problems linked with PCOS such as obesity, insulin resistance, dyslipidemia, diabetes and dysbiosis.
Even someone with normal weight may still have metabolic syndrome. Although waist circumference is one risk factor, there can be others like high blood pressure, high triglyceride, and high fasting glucose. Even just high fasting insulin with normal blood sugar could be a risk factor.
Another damaging dietary factor may be the high content of advanced glycated end products (AGEs) in food (Diamanti-Kandarakis E, 2012). AGEs are harmful compounds that are formed when protein or fat combine with sugar in the bloodstream. This process is called glycation. Diet is the biggest contributor of AGEs.
- The Gut:
The gut has recently been discovered to be linked to PCOS and its development. Research has found a clear association between changes in the gut microbiome and PCOS (Yurtdaş G, 2019).
Essentially, dysbiosis or unbalanced gut bacteria, due, for example, to a poor diet with a high-sugar intake, leads to leaky gut. Leaky gut causes an excessive immune system reaction that can interfere with insulin and drive up insulin levels. This leads to increasing testosterone produced by the ovaries, which interferes with normal follicle development and causes PCOS (Tremellen K, 2012).
- Hereditary Factors:
Exposure to high levels of androgens (or male hormones) in females during fetal development might result in long-term changes in gut microbiota in the daughters of PCOS patients (Zhang F, 2019). Prenatal androgen exposure can cause infant gut dysbiosis and altered abundance of bacteria, suggesting that androgen excess in immature fetuses could result in long-term alterations in gut microbiota and lead to increased risk of developing PCOS (Zhang F, 2019).
- Environmental exposure to industrial products:
Environmental toxins, especially, Bisphenol A (BPA), is thought to contribute to PCOS (Diamanti-Kandarakis E, 2012). Toxins, such as plasticizers, BPA and phthalates, act as endocrine disruptors in the development of PCOS (Diamanti-Kandarakis E, 2012).
Extensive exposure to environmental toxins and their role in contributing to PCOS are supported by extensive data (Rutkowska AZ, 2016). Acute or prolonged exposure to EDCs (endocrine disrupting chemicals) can disrupt hormones and reproductive function (Rutkowska AZ, 2016). They may also interfere with metabolic factors such as obesity, insulin resistance and hyperinsulinemia that can exacerbate the possibility of developing PCOS and contribute to PCOS in the form of type 2 diabetes and cardiovascular disease (Rutkowska AZ, 2016).
- Dysregulation of the sympathetic nervous system or HPA axis:
Dysregulation of the sympathetic nervous system may also act as an important component in PCOS (Shorakae S, 2015). Women with PCOS show increased rates of dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis (Peecher DL, 2019). The key clinical features of PCOS are anovulation, hyperandrogenism and hyperinsulinemia, which are closely related with a dysregulated endocrine system (Wang F, 2017).
Cortisol (as part of the HPA axis) dysregulation can also affect insulin levels, playing a role in the endocrine dysfunction in PCOS patients (Wang F, 2017).
——– To Be Continued Next Week ——-
Please stay tuned and read our next article on PCOS Part #2 where we will discuss solutions on how to manage and address PCOS using Functional Medicine. Thank you for tuning into this week’s article on the causes of PCOS.
Are You Suffering From A Chronic Illness?
Does your current health situation look like this…
- Do you feel that you have tried many things and either nothing works, or the treatment does not hold?
- Have you been told that there is nothing that can be done to reverse your illness and you just need to manage symptoms?
- Does your illness impact your work, your family, your happiness and your social life?
We specialize in finding answers and solutions for complicated chronic illness when people feel like they have tried everything. If this sounds like you, book a free call with us to see if we are the right fit for your health goals.
Dr. Miles has spoken for the following organizations:


















Responses