Is Lyme Disease Curable?
In this blog, we will focus on answering the question ‘Is Lyme Disease Curable?’. You will learn:
- What the basic approach to treating Lyme Disease is
- What the complications and obstacles to successful treatment are
- How we can apply Functional Medicine principles, look for the root causes and successfully treat & cure Lyme Disease
Do you suffer from fatigue, headaches or muscle or joint pain? Do you have Lyme Disease and on-going symptoms that you can’t seem to shake? Then this blog on Lyme Disease is for you. Please read on for the details!
** Please note: If you want the longer, more detailed version of this article, then please click here **
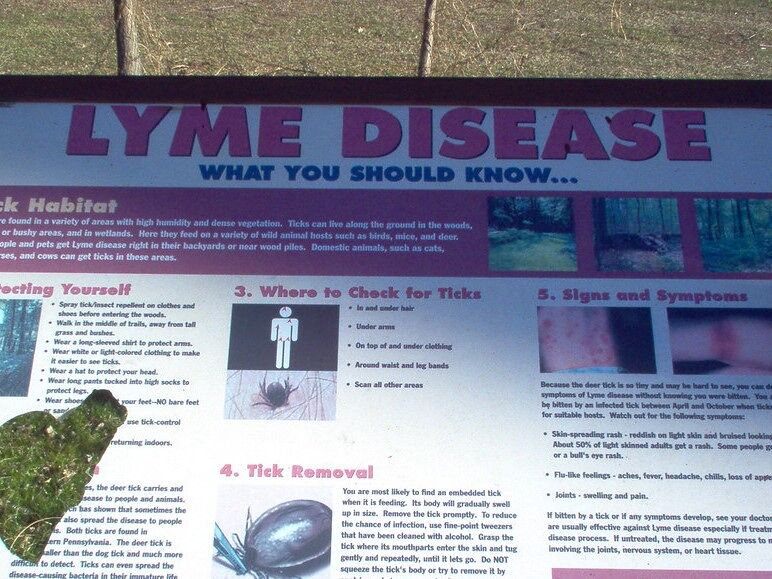
What is Lyme Disease (LD)?
Please refer to our article here for a detailed explanation of what Lyme Disease is. Between 2010 – 2018, there was an average of 476,000 LD diagnoses per year in the US (Maksimyan S, 2021). The incidence of Lyme Disease is rising.
To Read About Blog Topic, Scroll Down
Want To Work With Our Clinic?
Do you have a chronic or mystery illness that no one has been able to help you with? Are you simply wanting to re-connect with a healthier version of yourself? It’s Time To Finally Feel Better!
Is Lyme Disease Curable?
You can learn about how we treat Lyme Disease at our clinic HERE
- Lyme Disease is usually curable. It is best to catch it as early as possible. Seek medical advice as soon as you realize that you have been bitten by a tick, have a bull’s eye rash or suspect you may have been exposed to Lyme Disease after time in nature.
- If we apply our Functional Medicine principles and always search for the root cause(s), we can untangle, treat and cure most complex cases of Lyme Disease. In complicated cases, a deep dive to identify root causes will help to develop a multi-pronged treatment plan to improve, and likely resolve, symptoms.
Lyme Disease can be difficult to treat. The CDC estimates that 10 – 20% of patients who are properly treated for Lyme may remain symptomatic after treatment for a variable and unspecified length of time (Hout, 2018). Lyme Disease is rarely life-threatening, but delayed treatment can result in more severe disease.
Is Lyme Disease Curable? The Treatment Options
- Lyme Disease is typically treated with antibiotics. Conventional medicine will usually prescribe a 2–4-week course of oral antibiotics.
- It is also possible to treat Lyme more naturally with herbs and supplements.
- In our clinic, we use both natural and antibiotic treatments on a case-by-case basis.
- If correctly identified early on, most cases of Lyme Disease can be treated successfully with either herbal natural approaches or antibiotics.
Lyme Disease that goes misdiagnosed or untreated is more problematic. It can develop into a debilitating syndrome. In our clinic, we have expertise in treating a range of complicated, difficult-to-diagnose conditions like Lyme Disease. We look for the root causes in our patients to identify what could be causing the symptoms. We regularly treat and resolve Lyme, chronic infections and other complex conditions in patients in our Functional Medicine clinic.
Is Lyme Disease Curable? The Complications
You can learn about how we treat Lyme Disease at our clinic HERE
If not treated correctly and early on, Lyme symptoms can persist. Different variations of late-stage Lyme Disease include (Radolf JD, 2021):
- Late Neuroborreliosis
- Post Treatment Lyme Disease Syndrome
- Chronic Lyme Disease
Late Neuroborreliosis
In late neuroborreliosis, Lyme symptoms become neurological.
Conventional medicine typically uses antibiotics to treat patients with neurological signs of Lyme neuroborreliosis (Rauer S, 2018). The current recommendation is 2-3 weeks of antibiotics. There is not a lot of research on treatment. But the information does show that taking antibiotics for longer, by a further 100 days, showed no clinical advantage over a placebo (Rauer S, 2018).
In most trial studies, a 1–2-week course of antibiotics improved neurological symptoms in most patients within a few weeks to months (Rauer S, 2018). Lyme neuroborreliosis patients typically stabilized within one year after treatment.
But 60–80% of those with late neuroborreliosis can still experience lingering neurological symptoms (Rauer S, 2018).
That is a high proportion of patients who do not completely recover with conventional treatments. This is where Functional Medicine can help with a more targeted diagnosis and treatment plan.
Post Treatment Lyme Disease Syndrome (PTLDS)
In post-treatment Lyme Disease syndrome or PTLDS, patients have symptoms that persist after treatment. Symptoms include fatigue, pain and cognitive difficulties. These persist past the initial antibiotic treatment of acute LD, and last over six months or longer post-treatment (Maksimyan S, 2021).
PTLDS occurs in approximately 10% of patients with Lyme Disease, following antibiotic treatment (Fitzgerald BL, 2021). Researchers have not been able to identify why some people get PTLDS or what the predisposing factors are. It is also quite tough to diagnose, treat and prevent (Maksimyan S, 2021).
Long-term trials of antibiotics are the most researched treatment plans for PTLDS. Studies indicate that longer-term antibiotics for these persistent symptoms of LD have no additional benefits than a 2-week course of antibiotics (Maksimyan S, 2021).
One study from the late 1990s looked at whether post-LD symptoms, especially severe fatigue and slower mental speed, would improve with long-term antibiotics (Maksimyan S, 2021). The study found that antibiotics only improved some symptoms and may not be the right approach for every patient (Maksimyan S, 2021).
There may be adverse effects from longer antibiotic use (Maksimyan S, 2021). In one study, 73% of patients on antibiotics reported an adverse event. The most common events were rash, diarrhea and allergic reactions.
Once again, it is critical to get a correct diagnosis to avoid over-prescribing antibiotics (Maksimyan S, 2021).
How common is PTLDS?
One relatively small study showed 35% of participants had PTLDS, and that these patients had significantly lower function and quality of life within six months of treatment (Maksimyan S, 2021). This study specifically recruited patients with early-diagnosed LD who received immediate treatment.
Various medications have been trialed to treat PTLDS but so far none have been found to be effective (Maksimyan S, 2021).
One encouraging study looked at a non-pharmaceutical therapy for chronic Lyme disease: resistance training in patients. People with a previous LD diagnosis and symptoms persisting for at least three months after treatment were recruited. After a supervised 4-week resistance exercise training, they had significant improvement in their joint pain symptoms, exercise performance and the number of days they felt healthy and full of energy (Maksimyan S, 2021).
Chronic Lyme Disease (CLD)
CLD is when patients have unexplained, on-going symptoms. CLD can include a range of symptoms such as fatigue and chronic pain which occur due to a lengthy Borrelia infection.
Often, people don’t notice a tick bite or may not get a bulls-eye rash. They may not think of getting checked for Lyme and may have a long delay in getting a correct diagnosis. This can lead to chronic Lyme. Or their antibiotics treatment may not work, as it is not a fail-proof cure. Patients with chronic, long-standing Lyme Disease are often sick for long periods of time following treatment or may experience a worsening of their Lyme symptoms despite treatment (Shor S, 2019).
CLD Treatment
Additional or longer courses of antibiotics do not help patients after being treated the first time for Lyme (Halperin, 2015). Antibiotics are ineffective in patients with persistent fatigue and cognitive symptoms following appropriately diagnosed and treated Lyme disease (Halperin, 2015). This can even put patients at risk of side effects from the antibiotics (Halperin, 2015).
We would recommend that patients who have tried antibiotics and are still not cured look to Functional Medicine to find the underlying causes for symptoms and treat them with a more targeted approach than just antibiotics.
Co-Infections of Lyme Disease
We will look at Lyme Disease co-infections in another blog. It is an important topic and can affect the outcome and success of treatment. However, it is beyond the scope of this article so please stay tuned for a future blog on Lyme co-infections
Degenerative Neurological Diseases
Lastly, a great concern is when LD goes misdiagnosed or untreated. In these cases, LD can, years later, be diagnosed as chronic inflammatory age-related degeneration (for example arthritis, dementia or stroke). This is partially due to the increased complications of aging for those with persistent and untreated Lyme Disease.
Some neurological diseases can even be partially caused by Lyme Disease. We have written extensively about this and you can find the links to blogs here, including Lyme and Alzheimer’s.
Lyme Disease is usually curable. It is best to catch it as early as possible. It is critical to seek medical advice as soon as you realize that you have been bitten by a tick, have a bull’s eye rash or suspect you may have been exposed to Lyme Disease after time in nature.
As always, please get in touch with us. If you or someone you know is struggling with pain, fatigue or other issues related to Lyme Disease, contact our clinic today. We can work on any issue(s) and improve your health. Book a free health evaluation call with us today, to see how we can help you with your concerns. We can answer your questions and help you book an initial consult with one of the functional medicine doctors in our clinic.
** Please stay tuned for our next Blog! **
Are You Suffering From A Chronic Illness?
Does your current health situation look like this…
- Do you feel that you have tried many things and either nothing works, or the treatment does not hold?
- Have you been told that there is nothing that can be done to reverse your illness and you just need to manage symptoms?
- Does your illness impact your work, your family, your happiness and your social life?
We specialize in finding answers and solutions for complicated chronic illness when people feel like they have tried everything. If this sounds like you, book a free call with us to see if we are the right fit for your health goals.
Dr. Miles has spoken for the following organizations: