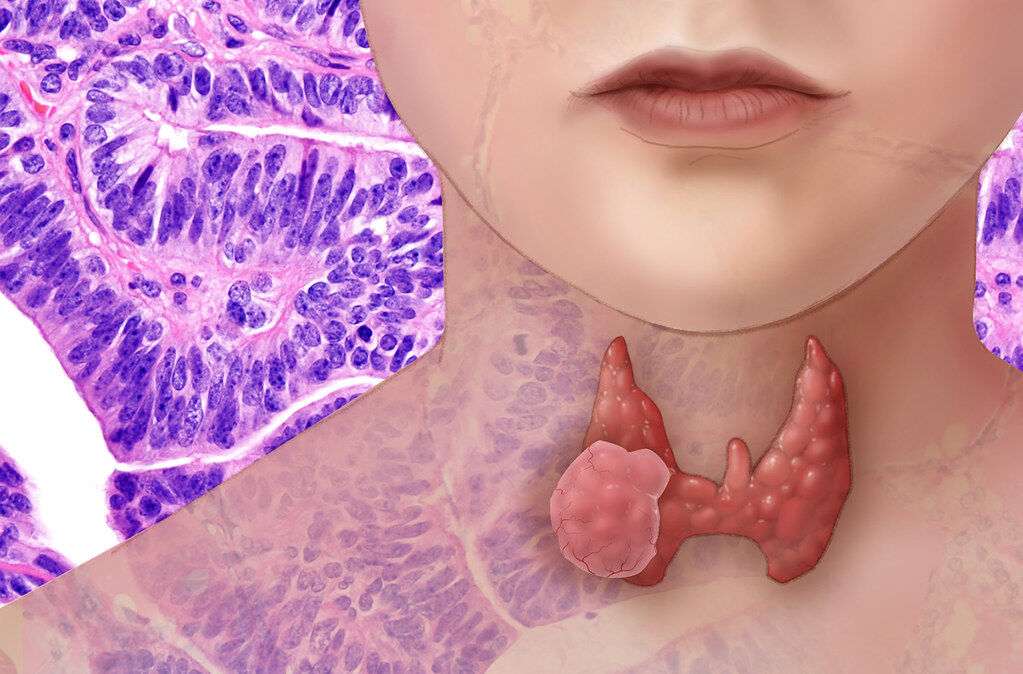
Graves Disease
Welcome to our Thyroid Series of blog articles. This article covers the root causes of Graves disease. Next week we will discuss Functional Medicine solutions to Graves. We hope you have followed our previous articles. In future articles in this series, we will look at other conditions of the thyroid and how to address each one.
** Please note: If you want the short summary version of this article with a video, then please click here **
GRAVES DISEASE is an autoimmune disorder that causes hyperthyroidism, or overactive thyroid. In Graves, the immune system makes antibodies that falsely act like TSH, causing the thyroid to create more thyroid hormone than needed. The immune system creates an antibody called thyroid-stimulating immunoglobulin (TSI) (National Institue of Health, 2020). TSI tells the thyroid to increase the production of thyroid hormones (National Institue of Health, 2020). Normal thyroid function is regulated by a hormone released by the pituitary gland. Thyrotropin receptor antibody (TRAb) is one of the antibodies associated with Graves disease. Sometimes TRAb acts like the pituitary hormone and interferes with the normal regulation of the thyroid, causing an overproduction of thyroid hormones (hyperthyroidism) (Mayo Clinic, 2020).
Graves affects 1% to 1.5% of the population (Wiersinga, 2019).
Approximately 3% of women and 0.5% of men develop Graves disease during their lifetime (Wiersinga, 2019). It is more common in women than in men due to hormonal factors (National Institue of Health, 2020). Another theory says that the gender difference is probably due to differences between male and female immune systems (Ferrari SM, 2017). Men have more immune suppression versus women so women show greater immune reactivity (Ferrari SM, 2017).
- Graves disease is the most common cause of thyroid overactivity (hyperthyroidism) (National Institue of Health, 2020).
- Having one autoimmune condition like Graves disease increases the risk of developing other autoimmune disorders, including rheumatoid arthritis, pernicious anemia, celiac disease, type 1 diabetes and others.
- Untreated Graves disease can lead to a number of issues including heart disorders, osteoporosis and ‘thyroid storm’ (American Thyroid Association, 2020). Thyroid storm is when a sudden and drastic increase in thyroid hormones cause accelerated hyperthyroidism or thyrotoxic crisis, requiring emergency medical attention (American Thyroid Association, 2020).
To Read About Blog Topic, Scroll Down
Want To Work With Our Clinic?
Do you have a chronic or mystery illness that no one has been able to help you with? Are you simply wanting to re-connect with a healthier version of yourself? It’s Time To Finally Feel Better!
SIGNS & SYMPTOMS OF GRAVES include:
- Pretibial myxoedema (lesions of the skin), as a result of thyroid disease
- Anxiety, nervousness
- Fatigue, muscle weakness
- Hair and nail changes
- Weight loss
- Increased heart rate
- Increased systolic blood pressure
- Heat intolerance
- Tremors
- Change in libido
- Increased temperature, sweating
- Frequent bowel movements
- Headaches
- Hives
- Nausea and vomiting
- Swollen lymph nodes
- Increased appetite
- Enlarged thyroid gland, called a goiter
- Bulging eyes or Graves ophthalmopathy: 25 to 50% of people with Graves disease have eye problems (National Institue of Health, 2020). This can include swelling and inflammation, redness, dryness, puffy eyelids, and a gritty sensation like having sand or dirt in the eyes. Bulging of the eyes is due to inflammation of tissues behind the eyeball and a retraction of the eyelids. On rare occasions, eye problems can be more serious and include pain, double vision and compression of the optic nerve connecting the eye and the brain, which can cause vision loss (National Institue of Health, 2020).
ROOT CAUSES of Graves:
All Health Begins in the Gut – Hippocrates
As an autoimmune disease, Graves is caused by the Triad of Autoimmunity (see here and here). The Triad of Autoimmunity is:
- A Genetic Tendency
- An Environmental Trigger
- A Leaky Gut
As an immune system issue, we need to review gut health and other impacts on immunity. The environmental triggers are different for each person but are likely to be gut imbalances, infections, nutritional deficiencies, toxic exposures and stress. With comprehensive lab testing used in FM and a detailed review of the patient’s history and environment, we can identify the individual root causes of a person’s case of Graves and address it using dietary and lifestyle changes.
GUT HEALTH: As an autoimmune disease, Graves is linked to poor gut health. Leaky gut, or intestinal permeability, is involved, as well as other possible GI problems. Our article here shows how leaky gut can lead to an overactivated immune system that can attack the thyroid gland.
These are the types of GI issues to look into:
Intestinal permeability or leaky gut: Tight junctions regulate the permeability of the gut, which is meant to remain ‘closed’ to the rest of the body. What you eat is digested, nutrients are absorbed through the gut lining and then the waste is excreted through the anus. What you put into your mouth is not meant to go directly into the bloodstream to circulate. If this happens and molecules, proteins and toxins can get into the blood circulation, then leaky gut exists. The immune system sees these unexpected molecules leaking through the gut lining as foreign invaders and mounts an immune response attack. Because the gut is leaky, this will happen over and over multiple times. The immune system eventually goes into high alert from so many invaders and becomes overactivated. It then starts to attack own tissue and the auto-attack of autoimmunity has begun. In the case of Graves, the immune system is attacking thyroid tissue. We must heal the gut to ‘close’ the leaky gut in order to stop the autoimmune attack.
Dysbiosis: Imbalanced gut flora or gut microbial dysbiosis (more bad gut bacteria than good bacteria) is also a risk factor for Graves (Ishaq HM, 2018). A disturbed microbiota composition increases the prevalence of Graves disease (Fröhlich E, 2019). Research shows there is less diversification of intestinal bacteria in Graves patients in contrast to controls (Ishaq HM, 2018). Certain species of gut bacteria are more prevalent in the guts of Graves patients (Ishaq HM, 2018). These microbes influence thyroid hormone levels by regulating iodine, selenium, iron and zinc, which affects overall thyroid health (Fröhlich E, 2019).
Gluten, molecular mimicry & celiac disease: Gluten is a well-known issue in autoimmune thyroid diseases. Gluten contributes to leaky gut, which is a predisposing factor for autoimmunity (read more here). Increased intestinal permeability due to gluten can lead to increased immune activation and production of antibodies which indicate autoimmune thyroid disease (Kassa W, 2020). This is thought to happen through molecular mimicry between gluten and thyroid tissue (Kassa W, 2020). In one case study, a patient with Graves resolved symptoms and improved thyroid function tests after switching to a gluten-free diet (Kassa W, 2020). Removing gluten from the diet has anti-inflammatory effects which help treat autoimmune conditions (Kassa W, 2020). The prevalence of celiac disease, another autoimmune condition, in patients with Graves is higher than in the healthy population. Celiac rates in people with Graves is 4.5% compared to only 0.9% in healthy controls (Kassa W, 2020).
Helicobacter pylori (H. pylori) infection: H. pylori infection is more common in people with Graves at 67% vs. 29% of controls (Figura N, 2019). H. pylori infection is associated with Graves through increased inflammation and molecular mimicry (Figura N, 2019). In one study on H. pylori and Graves, the blood levels of IL-6, an inflammatory marker, among H. pylori-positive patients was almost ten times higher than among controls (Figura N, 2019). This increase in proinflammatory cytokines in Graves patients indicates that pathogenic strains of H. pylori might initiate or amplify, or both, the autoimmune response (Figura N, 2019). In addition, the thyroid antigens most frequently used to diagnose and monitor Graves are Tg, TPO, and TSH-R, all of which are structurally similar to H. pylori bacterial proteins (Figura N, 2019). Molecular mimicry between the thyroid antigens Tg, TPO, and TSH-R and different H. pylori bacterial proteins exists. This cross-reactivity between anti-H. pylori antibodies and thyroid cells suggests molecular mimicry between the thyroid and these bacteria. This predisposes for an autoimmune attack on the thyroid when H. pylori is present (Figura N, 2019). Finally, H. pylori can contribute to leaky gut, which can lead to autoimmunity.
Anything else that leads to leaky gut is an issue for autoimmune thyroid disease, such as SIBO (Small Intestinal Bacterial Overgrowth), excess alcohol consumption or industrial food processing that can increase inflammation in the gut and potentially contribute to leaky gut. Other potential environmental triggers for Graves include infection, iodine, certain drugs, smoking and stress (Shukla SK, 2018).
Viral or bacterial INFECTIONS: Inflammation of the thyroid gland can occur as a result of a (typically viral) infection (EndocrineWeb, 2014). The infection can affect thyroid function, possibly cause thyroiditis and modify the production of thyroid hormones (American Thyroid Association, 2020). Epstein-Barr Virus, or EBV, is frequently found with autoimmune thyroid conditions. There is a significantly higher presence of EBV DNA copies in patients newly diagnosed with Graves, compared to the control group (Pyzik A, 2019). This suggests a very likely role of the EBV virus in the development of Graves (Pyzik A, 2019).
Viral infections include Epstein-Barr Virus, Lyme disease, herpes virus, hepatitis C virus, retroviruses, influenza B virus and others. Bacterial infections are Yersinia enterocolitica, Borrelia burgdorferi, a co-infection with Lyme disease, Helicobacter pylori which we previously discussed and others.
NUTRITION: Proper functioning of the thyroid gland requires a number of nutrients, including selenium, iodine, iron, zinc, D and others (Stuss M, 2017).
Excess iodine: The most common cause of hyperthyroidism is excess iodine intake (Shukla SK, 2018). The thyroid uses iodine to make thyroid hormone. How much iodine is consumed affects the amount of thyroid hormone made. Too much or too little iodine is a problem and it is important to get the correct amount. If someone with a relatively low intake of iodine suddenly consumes a very iodine-rich diet, over time that individual can produce an excessive amount of thyroid hormone, resulting in an overactive thyroid (Shukla SK, 2018). In someone with a predisposition to autoimmunity, this excess iodine can contribute to the development of Graves disease.
Vitamin D: A review of all studies found that Graves patients were more likely to be deficient in vitamin D (Ishaq HM, 2018). This can be a trigger for immune system dysfunction and Graves that contributes to the disease progression (Ishaq HM, 2018).
Selenium: Selenium suppresses part of the immune reaction, by inhibiting the inflammatory response (Stuss M, 2017). It protects the thyroid against oxidative stress and helps convert T4 into T3 (Stuss M, 2017). It can also mitigate the consequences of excess iodine, preventing excess inflammation in the thyroid (Stuss M, 2017). Lower selenium concentrations were found in patients with Graves disease (Stuss M, 2017).
Food sensitivities and inflammatory foods: Inflammatory foods and foods that you are sensitive to may lead to further inflammation and disease in the body. This can lead to the overproduction of antibodies, which may end up attacking your own body, including the thyroid gland.
TOXINS: The thyroid is very sensitive to environmental toxins. Iodine and selenium have an ‘affinity’ or a chemical attraction to thyroid tissue. This is helpful as these two minerals are required for thyroid hormone production. However, other molecules can have this same affinity. Unfortunately, many environmental toxins have molecular structures that are similar to thyroid tissue (or affinity with the thyroid). They are then mistaken for iodine and selenium by the thyroid, so they accumulate in the thyroid.
The toxins to look out for fall into four categories
- Heavy metals: aluminum, cadmium, lead and mercury
- Household toxins: Polybrominated diphenyl ethers (PBDEs) i.e. flame retardants, Bisphenol A (BPA), phthalates
- Industrial chemicals: dioxin, perchlorate, perfluorinated chemicals, or PFCs, and polychlorinated biphenyls, or PCBs
- Agricultural agents: pesticides containing organochlorine, herbicides and fungicides (Ferrari SM, 2017)
- Cigarette smoking is a key source of cadmium and affects the immune system. It can increase the risk of Graves disease (National Institue of Health, 2020). Smoking increases the risk of eye problems and is associated with more severe eye abnormalities (Graves ophthalmopathy) (National Institue of Health, 2020). The reason cigarette smoking increases Graves is due to the immune system modulation (Sawicka-Gutaj N, 2014). TSH is lower in smokers, while Free T4 and Free T3 are reported at higher levels in smokers compared to nonsmokers (Sawicka-Gutaj N, 2014).
Emotional STRESS: Recent studies suggest that psychosocial factors including emotional stress are related to the onset of Graves (Fukao A, 2019). Stress factors such as stressful life events, daily hassles and negative feelings, were found to be significantly higher in Graves patients vs. controls (Fukao A, 2019). Some studies did not find this to be the case (Fukao A, 2019). However, it is very difficult to quantify stress levels leading up to a disease diagnosis as it is both subjective and retrospective. The balance of research says that stressful life events may act as a trigger for the onset of Graves disease among people who are genetically susceptible (Fukao A, 2019).
TESTING FOR GRAVES
There are two antibodies to look for when testing for Graves. TSI (thyroid stimulating immunoglobulin) are antibodies that tell the thyroid to become more active and release excess amounts of thyroid hormone into the blood. If TSI is high, then the thyroid is overactive. Thyroid stimulating hormone receptor antibodies (TRAb) is the other antibody to check. In Graves disease, TRAb can mimic the action of TSH and cause hyperthyroidism. TRAb can also inhibit the action of TSH and cause hypothyroidism (American Thyroid Association, 2020). Thyroid peroxidase antibodies (TPOAb) and thyroglobulin antibodies (TgAb) are typical for Hashimoto’s, but may also be present in Graves disease.
STANDARD TREATMENT FOR GRAVES (Graves Disease Foundation, 2020)
- Anti-thyroid drugs inhibit production and/or conversion of the active thyroid hormone and relieve symptoms. Possible side effects of anti-thyroid drugs are skin rash, itching, hives, nausea, vomiting, heartburn, headache, joint or muscle aches, loss of taste and a metallic taste. Graves disease is usually treated with antithyroid drugs for 12 to 18 months (Struja T, 2017). However, 40 to 60% of patients typically have a relapse of hyperthyroidism after stopping anti-thyroid drugs (Struja T, 2017). In these cases, the more invasive treatments of surgery or radioactive iodine are usually recommended (Struja T, 2017).
- Total thyroidectomy is a surgery to remove the thyroid gland so it cannot overproduce thyroid hormone.
- Radioactive iodine(RAI) is given to destroy part or all of the thyroid gland so it cannot overproduce thyroid hormone.
Radioactive iodine therapy or surgery cause hypothyroidism, requiring thyroid medications for life.
According to conventional medicine, there is no ‘cure’ for Graves (Wiersinga W. , 2019). Medical guidelines state that the aim of a thyroidectomy or RAI treatment in Graves should be permanent hypothyroidism, requiring lifelong Levothyroxine medication to maintain thyroid function (Wiersinga W. , 2019). Creating a second disease in order to treat the original disease is not a cure (Wiersinga W. , 2019).
However, in Functional Medicine (FM), we cannot agree with this approach.It is entirely possible to stop the autoimmune attack on the thyroid. Depending on how far the condition has progressed, a case of Graves may be reversable or, at the very least, can be better managed with functional medicine, diet and lifestyle approaches.
** Please read our blog next week on **
Solutions to Graves disease using Functional Medicine
Are You Suffering From A Chronic Illness?
Does your current health situation look like this…
- Do you feel that you have tried many things and either nothing works, or the treatment does not hold?
- Have you been told that there is nothing that can be done to reverse your illness and you just need to manage symptoms?
- Does your illness impact your work, your family, your happiness and your social life?
We specialize in finding answers and solutions for complicated chronic illness when people feel like they have tried everything. If this sounds like you, book a free call with us to see if we are the right fit for your health goals.
Dr. Miles has spoken for the following organizations:
















Responses